Medical and Surgical Options to Restore and Maintain Scalp Hair

What causes scalp hair loss?
There are many causes for hair loss in men or women. However, in the overwhelming majority of males with hair loss, the cause is hereditary androgenetic alopecia, more commonly known as “male pattern baldness.” The presence of the hormone, dihydrotestosterone (DHT), in a genetically susceptible man, is necessary for this problem to occur. Similarly, for females most patients presenting with hair loss have hereditary female pattern hair loss. This condition is still being researched, but the hormone influences on hereditary hair loss in females may be different from those in males. Some of the less common causes of hair loss, which are reversible with treatment, include thyroid disease, iron deficiency, high fever, surgery or general anesthesia, “crash diets,” childbirth, and certain medications. There are also certain dermatologic scalp disorders that can result in temporary or permanent hair loss, such as lupus, lichen planopilaris, and alopecia areata. Many myths abound regarding this topic; hair loss is NOT caused by poor circulation, clogged hair follicles, frequent shampooing, the wearing of hats or helmets, or the presence of mites. It is also important to remember that most adults lose approximately 75–125 hairs from their scalps every day due to the natural process whereby some hairs go into a dormant state (telogen), and others come out of this state and begin to sprout a new hair (anagen).
As long as the process remains balanced, the number of hairs on the scalp remains constant. One other minor factor in hair loss is stress, which is thought to accelerate already genetically programmed hair loss. However, it probably does not cause hair loss by itself without the necessary genes and hormones.
The tendency for male and female pattern hair loss is genetically inherited from either side of the family and begins to develop after puberty. Hair on the scalp that is genetically susceptible to androgenetic alopecia (generally the front and top of the scalp), starts to shrink in its shaft diameter and potential length during each 3 to 5 year “life cycle,” until it eventually disappears. The hair on the back and sides of most men’s scalps is usually genetically “permanent” hair, which is destined to remain for that man’s lifetime.
What can be done about male pattern hair loss?
People with thinning hair now have more options available to them than ever before.
➣ Hair restoration surgery offers a permanent, living solution to lost scalp hair.
➣ Effective medical treatments are now offered in the form of a pill (finasteride) and a topical liquid (minoxidil). They require life-long treatment to maintain their effect.

➣ Cosmetic enhancers include colored creams, sprays, and powders that, when applied to the thinning scalp, help to camouflage thinning areas, as long as there is still some hair present in the area. They do not treat the hair loss process.
➣ Hairpieces are a non-surgical means to restore hair by covering bald areas of the scalp. There is a large variety of means for attaching these. The most common are glue adhesives, “weave” attachment, and clips.

Surgical Options: Hair Transplants—Follicular Unit Grafts and Multi- follicular Unit Grafts and Multi-Follicular Unit Grafts
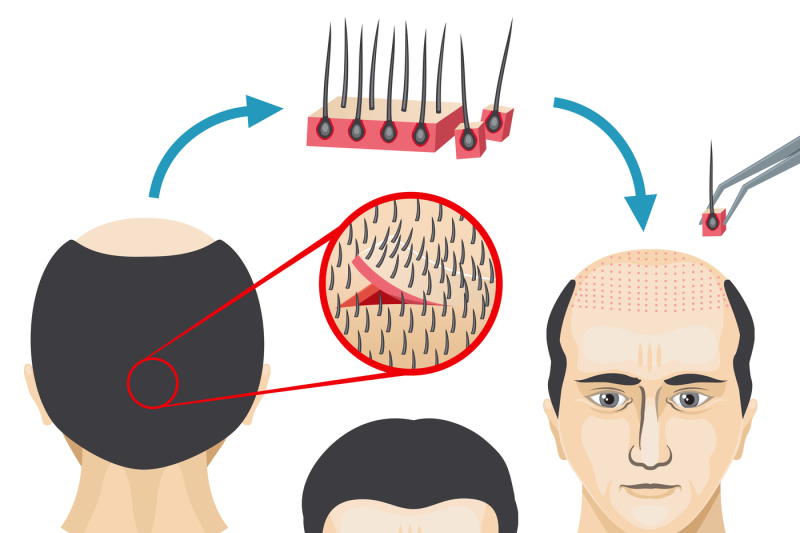
Modern techniques of surgical hair transplantation can restore lost hair and replace or re-shape your hairline with your own natural, growing hair, which needs no more care than the ordinary washing, styling, and trimming you have always done. Transplantation can be done today so well that often a barber or stylist cannot even tell that grafts have been placed. Hair transplantation involves removing permanent hair-bearing skin from the back and/or sides of the scalp (donor area). Then, using magnification, the tissue is dissected into follicular unit grafts (containing 1–4 hairs) and multi-follicular unit grafts (containing 3–6 hairs each).
Some surgeons prefer to transplant exclusively with follicular unit grafts, while others feel that placing the multifollicular unit grafts into the central areas of the scalp allows them to better create central density. Depending on the degree of balding in the frontal, mid-scalp, and vertex (crown) areas, usually 2–3 procedures are performed, with the number of grafts used varying tremendously, based on the area of potential alopecia, the patient’s “safe” donor supply, the textural characteristics of the patient’s hair, whether or not multi-follicular unit grafts are used in addition to follicular unit grafts, and the specific goals of the patient. Hair transplant surgery today is remarkably well tolerated. Within 24 hours small crusts will form on each graft that are then shed in approximately 4–14 days. The grafted hairs will often start to grow by 10–16 weeks after the procedure and will continue to grow for most, if not all, of one’s life. (As men and women age, in many there is a slight loss of hair density all over the head, which would naturally also affect the transplanted hairs). These small grafts are then meticulously planted into the bald or thinning area of the scalp (recipient area) so as not to injure any follicles already existing in the area and at the same exact angle as the other hairs present. The creation of very small follicular unit grafts has enabled the hair surgeon to create very natural, feathered hairlines, which do not have the abrupt, “pluggy look” that was commonly seen in hair transplants of years past.
What happens during a hair transplant procedure?
Hair transplantation surgery is considered to be “minor out-patient surgery.” Hair transplant procedures can take from 3–8 hours and are usually performed using local anesthesia on an out-patient basis, often with some supplemental oral or IV medication for sedation. Patients are often awake, but feel very relaxed because of the effect of the sedative. There is typically little discomfort during the surgical procedure. The donor areas, where the grafts have been harvested, are usually closed with sutures or surgical staples, except in the Follicular Unit Extraction technique, which does not require surgical closure.

These are usually removed in 7–14 days. Dissolvable sutures may occasionally be used in order to eliminate the need for you to return for suture removal. The recipient sites, where the grafts are placed on top, are essentially small, superficial needle holes or slits in the skin of the scalp. The surgeon should be willing to discuss with you the pros and cons of the various methods of both donor harvesting and transplanting the grafts. At the end of the procedure, either a very light dressing is applied, or, in many cases, the doctor will have you stay for brief observation and then allow you to leave with no dressing whatsoever. At the conclusion of the procedure the surgeon usually checks the final placement of the grafts, and the doctor or an assistant then explains the postoperative instructions, which are usually supplied in written form as well.

Who can benefit from hair restoration surgery?
Anyone who has experienced permanent hair loss may be a candidate for hair restoration surgery, including:
➣ Men with male pattern baldness
➣ Women with female pattern hair loss
➣ Men or women who want to restore or change the shape of their hairline
➣ People with areas of scarring from injuries or “scarring” skin diseases, and also patients who experienced some hair loss after surgery, such as face lift procedures
➣ People who want to thicken or restore eyebrows, eyelashes, and beards
➣ Men and women who want hair in an area where they have little or no hair
What happens after hair transplant surgery?
Hair transplantation is a very safe, relatively minor surgical procedure. Significant complications are extremely rare. There is usually little or no discomfort in the grafted area. Most patients feel some “tightness” in the donor area for 1–2 days and are prescribed a mild analgesic to help cope with this. Patients may be asked to use moist compresses or sprays and to sleep in a semi-upright position for 2–3 days following the procedure to minimize swelling and bruising. Small crusts may form on each graft, and these can usually be camouflaged by any existing hair that can be combed over the recipient area, or with camouflage products such as DermMatch, Couvre, or Toppik.

These crusts will flake-off by 5–14 days after the surgery, the smaller follicular unit scabs often falling off at 4–6 days and the multi-follicular unit scabs taking longer. The transplanted hair seen growing out of the scalp may initially be shed; however, the roots remain and will be dormant for 10–14 weeks, at which time the new hairs will all begin to grow. Numbness that may occur in the donor or recipient area usually disappears within 2–8 months following surgery. As stated above, complications are rare. Minor inflammation can occasionally occur around a newly transplanted hair follicle, similar to an infected ingrown hair or pimple, and usually responds to simple warm compresses. The scar that occurs in the donor scalp as a result of the removal of donor skin is usually quite narrow and can be easily hidden by the surrounding hair. The graft sites in the recipient frontal area heal with almost no visible scarring and are covered by the transplanted hair. A minority of patients may experience mild swelling in the forehead area for a few days following surgery. It typically appears around the 3rd post-op day and goes away after 3–4 days. Infection in either the donor or recipient area is extremely rare. Many patients experience a small area of numbness above the donor scar and in the rear central scalp that gradually disappears after a few months.

When should I start treatment?
Most doctors today recommend beginning medical treatment of significant hair loss as soon as the problem has been identified. Even if a patient decides to proceed with surgical hair restoration, medical treatment may slow or prevent additional hair loss in the future. Patients may have hair restoration surgery at any age after the early 20s, but the decision for any given patient may be different, depending on a number of factors. The vast majority of patients have their first procedure while they are not yet completely bald, so that they can use existing hair to help camouflage the procedure.
However, because hair loss tends to be both gradual and progressive, it is often unwise to start surgical treatment in a patient who is too young. Medical treatments such as finasteride and minoxidil are usually recommended for men with hair loss to help preserve or partially reverse thinning hair in the rear crown and in the area on top. Hair transplants can be used to fill in the front hairline and thicken the front half of the scalp, and medical treatments can be used to maintain hair behind the transplants and to possibly enhance the long-term results of hair restoration surgery. Your hair restoration surgeon will work with you to design an individualized plan to fulfill your specific needs.

How do I know if I am a good candidate for hair restoration surgery?
The elements that a doctor assesses to determine whether a candidate is a good subject for surgical hair restoration include such things as: the patient’s general state of health; the hair’s texture—fine or coarse; the contrast between the patient’s hair color and skin color; the density, i.e., the number of hair follicles per square inch of the hair in the donor area; the size of the area to be covered; the size of the area of donor hair; whether or not previous grafting procedures have been done; and the patient’s goals and expectations.
Making an accurate diagnosis and making treatment recommendations require an examination by a doctor and a frank discussion of possibilities between the patient and the doctor. The doctor should also give the patient a realistic estimate of the total cost of the planned procedure or procedures. The patient must understand that transplantation redistributes existing hair follicles and cannot create new hair follicles
What are the current medical treatments available?
Finasteride (Propecia®), an oral medication available by prescription only, has been introduced to the market in the past decade. Finasteride is approved only for use by men. Through scientific studies, it has been shown to re-grow hair in a significant number of men and stop hair loss in an even higher percentage. Finasteride works by decreasing the formation of DHT, a hormone responsible in large part for male pattern hair loss, while not reducing testosterone, the overall male hormone responsible for masculinity.
Finasteride (Propecia) works best for early or moderate hair loss, but it may also help patients with more advanced hair loss to preserve their remaining hair, and its use is suggested by hair restoration surgeons as an effective medication to slow down or reverse male pattern hair loss in many men. It is often used as a complementary treatment for hair transplant patients. Topical minoxidil (Rogaine®) has been around for over 15 years and is helpful in slowing down hair loss, but less effective in helping new hair to grow. A higher concentration (5% solution) of minoxidil is now available for men and has been shown to be more effective than the 2% solution. 5% minoxidil solution is generally not recommended for use by women because it may stimulate the growth of facial hair, and also because at least one study suggests that it is not more effective than the 2% in females. Both finasteride and minoxidil must be used on a continual basis in order to sustain results, and if discontinued, the process of balding resumes. These medications may not work for everyone, but they have a proven track record that shows a significant benefit to many people. In addition, combination treatment with minoxidil solution and finasteride may provide added benefit for men with androgenetic alopecia

How do I find a qualified hair restoration surgeon?
BabyFace MedSpa is now working closely with a doctor who has over 40 years of experience in hair recovery and transplant treatments and a team of excellent technicians to provide the best solution for our valued clients. We will be one of the best of its kind devoted to the advancement of knowledge and techniques pertaining to hair restoration surgery.
Please call BabyFace MedSpa at 905-554-7717 or E-mail us at [email protected] to book a complimentary consultation with our doctor and his assistant.
No particular technique or treatment is endorsed by BabyFace. A combination of techniques may be in the patient’s best interest. Excellent results can be produced using different techniques. The choice of a treatment regimen for any individual should be determined by consultation between that patient and our knowledgeable doctor.






